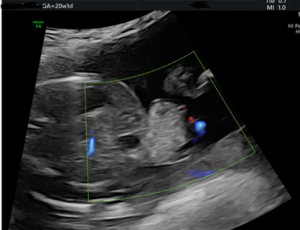
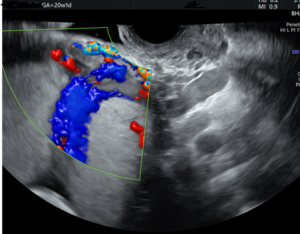
A patient with multiple high-risk factors—including advanced maternal age, an IVF pregnancy with a donor egg, and a history of four prior Cesarean deliveries—was referred for a 20-week anatomy scan. Ultrasound revealed several significant findings: an omphalocele, a persistent right umbilical vein, a suspected cardiac abnormality, and complete placenta previa with concern for placenta accreta.
Further evaluation through fetal echocardiography and amniocentesis confirmed tricuspid atresia with tricuspid regurgitation and A-wave reversal in the ductus venosus—a pattern consistent with compromised cardiac function. By 25 weeks, the fetus developed ascites, indicating worsening hemodynamics.
As the cardiac condition declined, the prognosis remained unfavorable. The patient began weekly biophysical profiles and hydrops surveillance, during which ascites progressed and polyhydramnios developed. At 27 weeks, the patient was admitted to the hospital for excessive vaginal bleeding related to suspected placenta accreta, where she remained under close care and continuous monitoring until delivery.
Despite these layered maternal and fetal complications, the care team successfully managed the pregnancy to 34 weeks and 1 day, greatly improving the baby’s chance of survival. Postnatal genetic testing confirmed Beckwith-Wiedemann syndrome, with a positive long-term outlook. Due to complications from placenta accreta, the patient underwent a hysterectomy at the time of delivery.
This story serves as a powerful reminder that diagnostic precision and compassionate collaboration are essential in shaping the outcome of even the most challenging cases. BB Imaging understands the clinical complexity and emotional gravity of managing high-risk pregnancies, which played a crucial role in providing expert ultrasound assessment, identifying structural anomalies, offering ongoing perinatal surveillance, and supporting maternal-fetal safety.